Connected Healthcare Data: Interoperability to Solve Fragmentation and Drive Better Patient Outcomes
May 26, 2022 | Updated: March 14, 2025
Many differences exist across healthcare systems around the globe, but there is one unfortunate similarity: fragmentation. Fragmentation is a consequence of the inability of various healthcare organizations (both public and private) to communicate with each other or to do so in a timely or consistent manner, and it can have a dramatic impact on patient and population well-being.
Interoperability and communication
A patient can visit a specialist for a specific condition and the family doctor for regular checkups, perhaps even on the same day. But how can both doctors make appropriate decisions if patient data is not shared between them?
Fragmented healthcare delivery, as described in this scenario, also leads to data fragmentation. Such data fragmentation can cause misdiagnosis and services duplication. It can also lead to billing issues, fraud, and more, causing preventable harm and representing a massive economic burden for healthcare systems worldwide.
To improve healthcare fragmentation, we need truly interoperable health data.
The longitudinal patient record
A longitudinal patient record (LPR) is a full, life-long view of a patient’s healthcare history and the care they’ve received. It’s an electronic snapshot of every interaction patients have, regardless of provider and service. Ideally, this record can be shared across any or all entities within a country’s healthcare system. The LPR represents a step beyond the electronic health record, extending past a specific healthcare network to a regional or national level.
It’s critical that LPRs use the same data format and structure to guarantee the ability of healthcare providers to easily and quickly interact with them. Data standards for LPRs are key to interoperability and can help address healthcare fragmentation, which, in turn, can help save lives by improving care.
FHIR
Fast Healthcare Interoperability Resources (FHIR) is a commonly used schema that comprises a set of API and data standards for exchanging healthcare data. FHIR enables semantic interoperability to allow effective communication between independent healthcare institutions and essentially defines “how healthcare information can be exchanged between different computer systems regardless of how it is stored in those systems” (ONC Fact Sheet, “What is FHIR?”).
FHIR aims to solve the fragmentation problem of the healthcare system by directly attacking the root of the problem: miscommunication.
As is the case for many other modern communication standards (for example, ISO 20022 for finance), FHIR builds its REST API from a JSON schema. This foundation is convenient, considering most modern applications are built with object-oriented programming languages that have JSON as the standard file and data interchange format. This approach also makes it easier for developers to build applications, which is perhaps the most important point: The future of healthcare delivery may increasingly depend on the creation of applications that will transform how patients and providers interact with healthcare systems for the better.
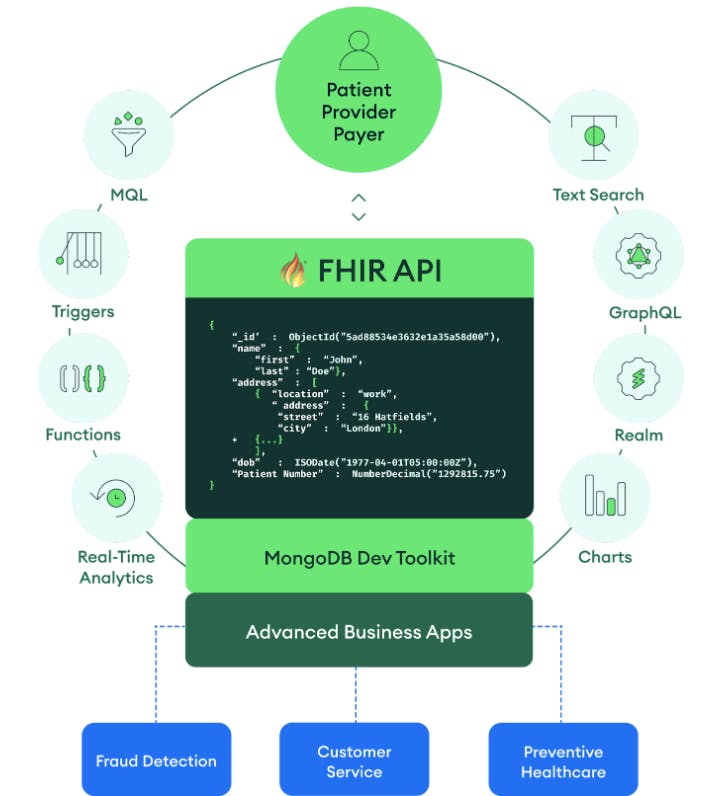
MongoDB: FHIR and healthcare app-ification
MongoDB is a document database and is therefore a natural fit for building FHIR applications. With JSON as the foundation of the MongoDB document model developers can easily store and retrieve data from their FHIR APIs to and from the database, with no translation or change of format needed. In fact, organizations can adopt FHIR resources as the basis of a new, canonical data model that existing internal systems can begin to shift and conform to.
One example is the Exafluence FHIR API, which is built on top of MongoDB. Exafluence's API allows for real-time data interchange by leveraging Apache Kafka and Spark, in either an on-premise or multi-cloud deployment. Software teams leveraging the Exafluence solution have experienced velocity increases of their FHIR interoperability projects by 40% to 60%.
Beyond FHIR, the trend toward healthcare app-ification (i.e., the increasing use of applications in healthcare) clashes with pervasive legacy architectures, which typically are not optimized for the developer experience. Because of this reliance on legacy architectures, modernization or transformation initiatives often fail to take hold or are postponed as companies perceive the risks to be too high and the return on investment is not evident.
It doesn’t have to be this way, however. MongoDB’s industry-proven iterative approach to modernization reduces the risk of application and infrastructure migration and unlocks developer productivity and innovation.
Interoperable, modern healthcare applications can now be built in a developer-friendly environment, with all the benefits expected from traditional databases (i.e., ACID transactions, expressive query language, and enterprise-grade security). MongoDB provides the freedom for solutions to be deployed anywhere (e.g., on-premises, multi-cloud), providing a major advantage for healthcare organizations, which typically have multi-environment deployments.
Healthcare and the cloud
Digital healthcare will accelerate the adoption of cloud technologies within the industry, enabling innovation at scale and unlocking billions of dollars in value. Healthcare organizations, however, have so far been reluctant to move workloads to the cloud, mostly because of data privacy and security concerns.
To support such cloud adoption initiatives, MongoDB Atlas offers a unique multi-cloud data platform, integrating MongoDB in a fully managed environment with enterprise-grade security measures and data encryption capabilities. MongoDB Atlas is HIPPA-ready and a key facilitator for GDPR compliance.
A holistic view of patient care
Interoperable healthcare records and communication standards will make longitudinal patient records possible by providing a much-sought-after holistic view of the patient, helping to fix healthcare fragmentation. Many challenges still exist, including transforming legacy infrastructures into modern, flexible data platforms that can adapt to the exponential changes happening in the healthcare industry. MongoDB provides a modern database designed to unlock developer productivity and ultimately giving healthcare organizations the power to focus on what matters most: the patient.
Read Part 2 of this series on connected healthcare data, and learn more about MongoDB Atlas and the healthcare industry.